By Wyatt Myers Medically reviewed by Cynthia Haines, MD everyday HEALTH
If you have fibromyalgia, you're undoubtedly familiar with the chronic pain and fatigue that often accompany this disorder — which affects about 5 million Americans, primarily women.
But feelings of pain and exhaustion aren't the only symptoms of fibromyalgia. Other signs that aren’t necessarily visible to others can affect you and make the condition even harder for those around you to understand.
Here are some of the lesser-known signs of fibromyalgia that you may experience:
Allodynia. You might not give a second thought to rubbing a loved one’s shoulders or patting a friend on the back. But for someone with allodynia, being the recipient of these simple gestures can result in excruciating pain. Allodynia is a heightened sensitivity to touch, which results in pain from things that normally would not cause discomfort.
“This increased skin sensitivity and pain from touch is hypothesized to occur for a number of reasons,” says Jacob Teitelbaum, MD, medical director of Fibromyalgia & Fatigue Centers. “Over one-third of people with fibromyalgia develop a small fiber neuropathy caused from the chronic pain. In addition, the chronic pain causes amplification of pain signals in the brain itself, as well as changes in three key neurotransmitters related to pain.” Dr. Teitelbaum says medications known as NMDA receptor antagonists — memantine (Namenda) is one — can help.
Allodynia is also related to a lack of restorative sleep, so standard treatments for fibromyalgia — such as physical therapy, exercise, stress relief techniques, and practicing good sleep hygiene — can also help ease allodynia.
Sensitivity to fragrance. This fibromyalgia symptom is almost directly tied to allodynia and occurs for many of the same reasons. “Increased light, sound, and smell sensitivity are all common,” says Teitelbaum. “We have an enormous amount of sensory input coming in, and it takes energy to sort through all of this to separate the noise from the static. Fibromyalgia predominantly represents an energy crisis, and as the body has trouble sorting through the signal from the noise, it reflects as increased sensitivities.” In addition to whole-body approaches to treating fibromyalgia, Teitelbaum says the anti-seizure medication gabapentin (Neurontin) can often help decrease these sensitivities.
“Fibro fog.” Also called “brain fog,” this is a very serious fibromyalgia symptom that leaves many people in distress. “Brain fog or fibro fog is a classic component of the energy crisis we call fibromyalgia,” says Teitelbaum. Some of the common signs of fibro fog include a difficulty with word finding or substitution, loss of short-term memory, and occasionally even episodic disorientation that lasts for about 30 to 60 seconds. "With this disease, calling one’s husband by another man's name is not a Freudian slip," Teitelbaum notes. He explains that there is no single cause for fibro fog; rather, it can be caused by a combination of many factors including low thyroid levels, poor sleep, hidden infections such as Candida, and alterations in blood flow to the temporal lobes of the brain, which regulate speech.
Stephen Soloway, MD, a rheumatologist in private practice in Vineland, N.J., attributes much of the difficulties with fibro fog to sleep issues affecting people with fibromyalgia. Practicing good sleep hygiene and getting help from a sleep specialist may be useful.
Paresthesia. Paresthesia is an unexplained feeling of tingling and numbness that people with fibromyalgia may experience. Often it's related to anxiety or nervousness over the disorder and can be accompanied by rapid, deep breathing. This in turn can lead to acroparesthesia, a tingling in the hands and feet from lack of carbon dioxide. Considering that anxiety is a major player in parasthesia, the stress relief techniques recommended for fibromyalgia patients can help. Exercise can also play a role in treatment.
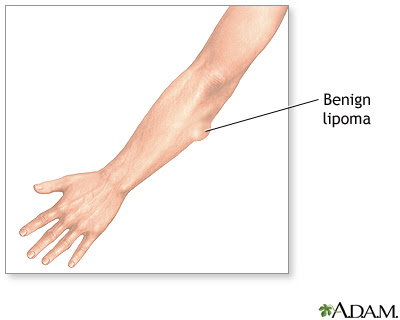
Lipomas. These benign fatty tumors that can appear as lumps in various parts of the body are not directly related to fibromyalgia, but they may cause you to experience more discomfort than the average person does. This may be related to where the lipomas develop — parts of the body that are susceptible to the excessive or inappropriate pain that patients experience, explains Elliot Rosenstein, MD, director of the Institute for Rheumatic and Autoimmune Diseases at Overlook Medical Center in Summit, N.J. “Alternatively, these may be fibro-fatty nodules or localized areas of muscle spasm.”
Excessive sweating. Some people with fibromyalgia perspire heavily and may even believe they have a fever. This is due to what’s called an autonomic dysfunction within the hypothalamus, the almond-sized area in the brain that controls sleep and regulates sweating, bowel movements, and other automatic body functions. “The autonomic dysfunction causes the increase in sweating," Teitelbaum says. Some medications and lifestyle changes that can keep you cool and dry may help with this fibromyalgia symptom.
Many of these unusual fibromyalgia symptoms respond to general treatment approaches. If not, talk with your doctor about targeted recommendations that may help.




















.png)





