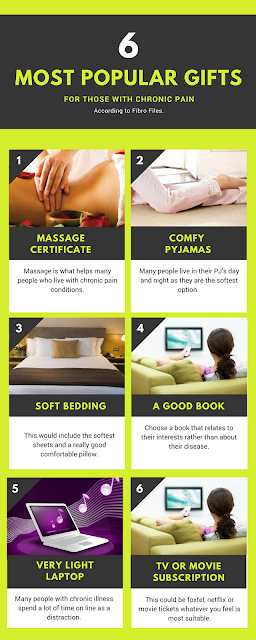
As someone with chronic illness myself I know that my number one gift to receive is a massage certificate especially from a practitioner who knows about myofascial release techniques which always help my tight painful muscles.
I wanted to see what others were recommending so I have researched quite a few different recommendations which I have linked to here. These lists include pillows, heated foot spas, body pillows, aromatherapy oils and diffusers, nerve-stimulating machines, kitchen gadgets, vitamins, humidifiers, heated blankets, first aid kits, ice packs and heated seat covers:
- Top 10 Gift Ideas under $100 for Chronic Pain Patients by Living With Fibromyalgia
- 2017 Fibromyalgia Gift Guide from Fed Up With Fatigue
- Christmas Gift ideas for chronic pain from Brainless Blogger
- Top eight Christmas gifts for people suffering from fibromyalgia and chronic pain by Back Pain Blog
- Gift Ideas for those with Chronic Pain at Fibro Fridays
- Top Christmas Gift Ideas for People with Chronic Pain at Pain Camp
- 10 Best Gifts for People with Chronic Pain at Community Pain Center
- Great gift ideas for a chronic pain sufferer from Pain Pathways Magazine
- 10 Gifts for the Person With Chronic Pain in Your Life at The Mighty
- Top 8 gifts for people with chronic pain from FibroMapp
- 9 Thoughtful Gifts For Someone With Chronic Pain at Prevention
- Video Reviews of Gift Ideas for Chronic Pain Patients by Living With Fibromyalgia
- Christmas Gift Ideas at In Spite of My Illness
- Christmas Gift Ideas For Spoonies at Living Creatively With Fibromyalgia
Many of these list suggestions are selling products on Amazon or elsewhere like relaxation CD's








.png)

.png)